What Is A Prior Authorization

What Is Prior Authorization And Importance Of Prior Authorization Prior authorization means that a health provider needs to get approval from a patient’s health plan before moving ahead with a treatment, procedure, or medication. Prior authorization is the approval from your health insurance that may be required for a service, treatment, or prescription to be covered by your plan if it's not an emergency.
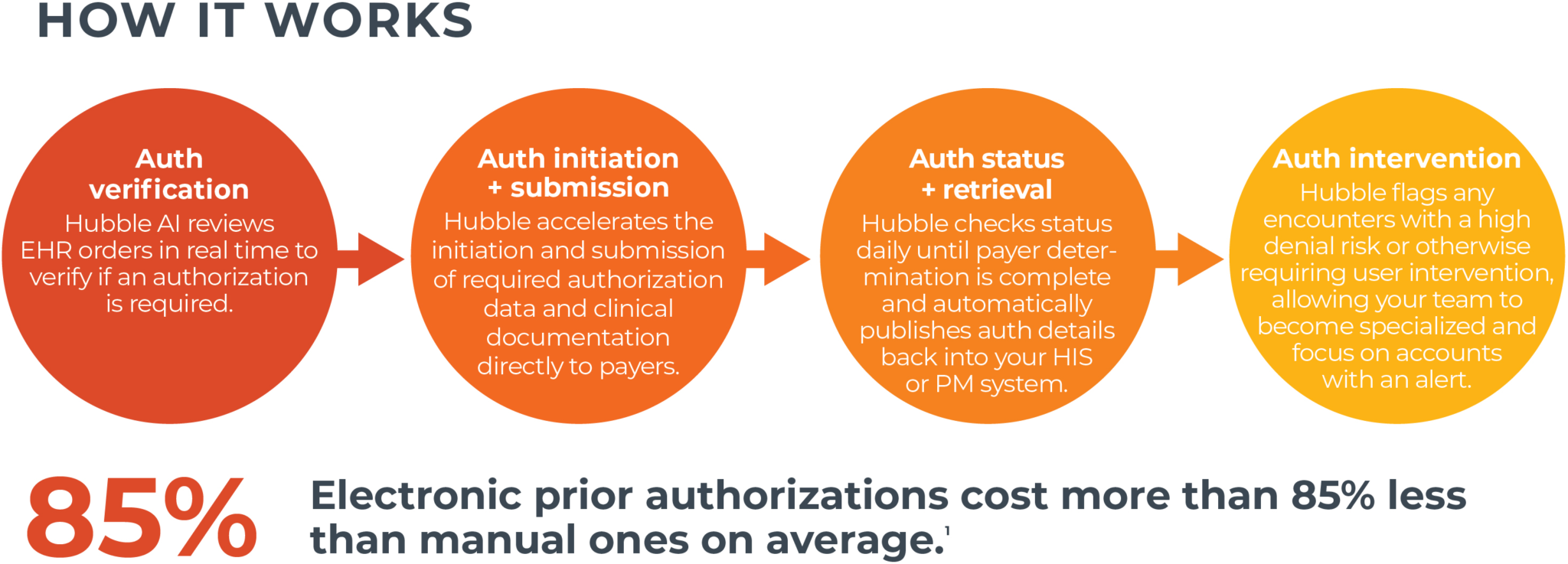
Prior Authorization Software Ai Powered Automated Waystar Prior authorization is an approval of coverage from your insurance company — not your healthcare professional. it’s a restriction put in place to determine whether or not they will pay for certain medications. Prior authorization, also known as preauthorization, preapproval, or precertification, is a process where a provider must get approval from your insurance company before insurance will cover a prescribed medication, procedure, or treatment. Prior authorization, also known as pre authorization or pre certification, allows health insurance plans to review proposed care ahead of time, confirm that coverage for the service is available under the plan, and give the medical provider approval to go ahead with the procedure or prescription. What is prior authorization? answer: prior authorization is a health plan policy that requires your physician to seek approval from your health plan before you can access a servi. e or prescription medication. this process applies to patients of all . ges, from infants to seniors. question: why do health insurance companie.
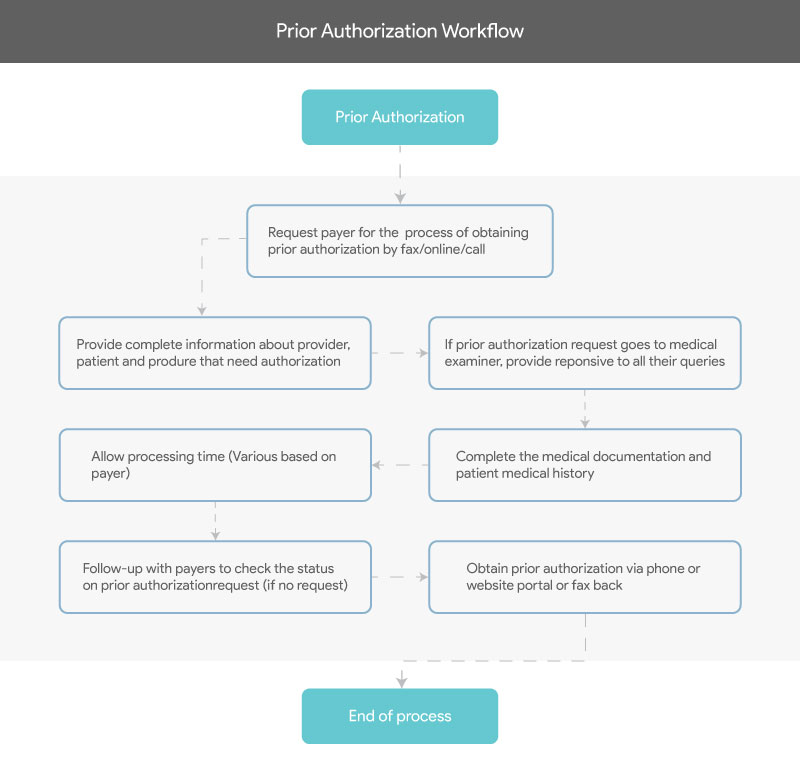
5 Key Strategies To Effectively Streamline And Overcome Prior Prior authorization, also known as pre authorization or pre certification, allows health insurance plans to review proposed care ahead of time, confirm that coverage for the service is available under the plan, and give the medical provider approval to go ahead with the procedure or prescription. What is prior authorization? answer: prior authorization is a health plan policy that requires your physician to seek approval from your health plan before you can access a servi. e or prescription medication. this process applies to patients of all . ges, from infants to seniors. question: why do health insurance companie. Under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. prior authorization is usually required if you need a complex treatment or prescription. coverage will not happen without it. In this guide, we will explain what a prior authorization is, why it matters, and how the process typically works. what is a prior authorization? a prior authorization is a formal approval from your health insurance company before you receive a specific medical service, medication, or procedure. Prior authorization (pa), also called preauthorization or precertification, is a requirement set by your health insurance provider. it means your doctor or healthcare provider must get approval from your insurer before moving forward with a specific treatment, procedure, test, or medication. When you’re dealing with a health issue, the last thing you need is a surprise bill for care you thought was covered. that’s why understanding the prior authorization process is key to your health care.

Prior Authorization Criteria Key Guidelines Explained Under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. prior authorization is usually required if you need a complex treatment or prescription. coverage will not happen without it. In this guide, we will explain what a prior authorization is, why it matters, and how the process typically works. what is a prior authorization? a prior authorization is a formal approval from your health insurance company before you receive a specific medical service, medication, or procedure. Prior authorization (pa), also called preauthorization or precertification, is a requirement set by your health insurance provider. it means your doctor or healthcare provider must get approval from your insurer before moving forward with a specific treatment, procedure, test, or medication. When you’re dealing with a health issue, the last thing you need is a surprise bill for care you thought was covered. that’s why understanding the prior authorization process is key to your health care.
Comments are closed.