Prior Authorization Verification Automation Automate Your Rcm
Automated Prior Authorization Solutions Agentic Ai Rpa WeInfuse and SamaCare are building a seamless integration to automate the prior authorization process for infusion providers across the country DALLAS, May 9, 2023 /PRNewswire/ -- WeInfuse, the Blue Shield of California partners with Salesforce to automate prior authorization The collaboration comes amid controversy about claims automation technology Paul Markovich, CEO of Blue Shield

Prior Authorization Verification Automation Automate Your Rcm A 2024 survey from the American Medical Association showed that 93% of physicians say prior authorizations lead to care delays for patients — and that 1 in 4 say prior authorization has led to a Blue Shield of California is partnering with tech company Salesforce to give physicians and patients prior authorization answers in actual time, instead of days The aim is to streamline the prior Health Tech Availity picks up Olive AI's payer-facing business as automation startup shifts focus to RCM solutions By Heather Landi Apr 11, 2023 7:30am Olive mergers and acquisitions Availity A survey of health plans finds prior authorization processes need improvement to become fully electronic While the healthcare industry is moving towards automation as a whole, prior authorization

Prior Authorization Verification Automation Automate Your Rcm Health Tech Availity picks up Olive AI's payer-facing business as automation startup shifts focus to RCM solutions By Heather Landi Apr 11, 2023 7:30am Olive mergers and acquisitions Availity A survey of health plans finds prior authorization processes need improvement to become fully electronic While the healthcare industry is moving towards automation as a whole, prior authorization An electronic health record tool has demonstrated the potential to automate the selection of biosimilarsBiosimilars are projected to reduce spending on biologic drugs in the United States by an About Availity Availity empowers payers and providers to deliver transformative, patient-centered healthcare experiences by enabling the seamless exchange of clinical, administrative, and ZeOmega®, the leading population health and interoperability technology company, today announced it was selected by the Massachusetts Health Data Consortium (MHDC), a nonprofit advancing health These tests represent a disproportionately high number of prior authorization clinical reviews, and Utilization Management (UM) teams struggle to keep current with new tests, rapidly evolving

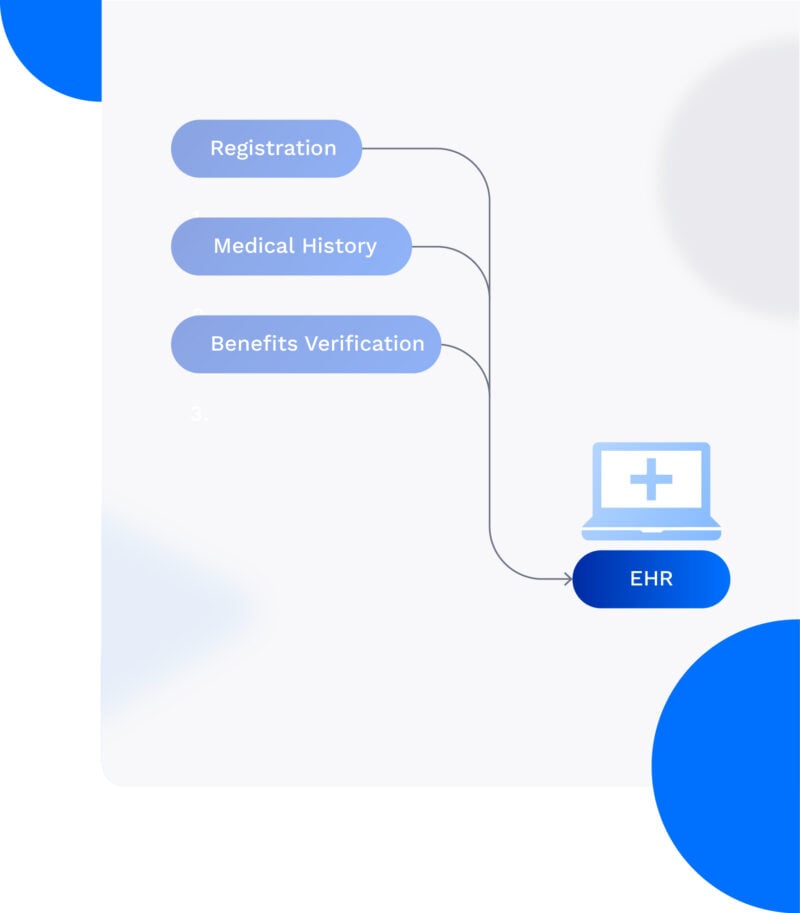
Automating Benefit And Eligibility Verification In Rcm An electronic health record tool has demonstrated the potential to automate the selection of biosimilarsBiosimilars are projected to reduce spending on biologic drugs in the United States by an About Availity Availity empowers payers and providers to deliver transformative, patient-centered healthcare experiences by enabling the seamless exchange of clinical, administrative, and ZeOmega®, the leading population health and interoperability technology company, today announced it was selected by the Massachusetts Health Data Consortium (MHDC), a nonprofit advancing health These tests represent a disproportionately high number of prior authorization clinical reviews, and Utilization Management (UM) teams struggle to keep current with new tests, rapidly evolving
Comments are closed.