Is Prior Auth Automation The Key To Improved Financial Performance One

Is Prior Auth Automation The Key To Improved Financial Performance One Prior authorizations are a critical part of the revenue cycle as they impact both reimbursement and patient access to care, and automation may help simplify the process. For the 78% of respondents who report improved financial performance, key outcomes include a more efficient, streamlined authorization process; decreased time to approval (within 24 hours); and fewer denials being sent back to provider organizations.
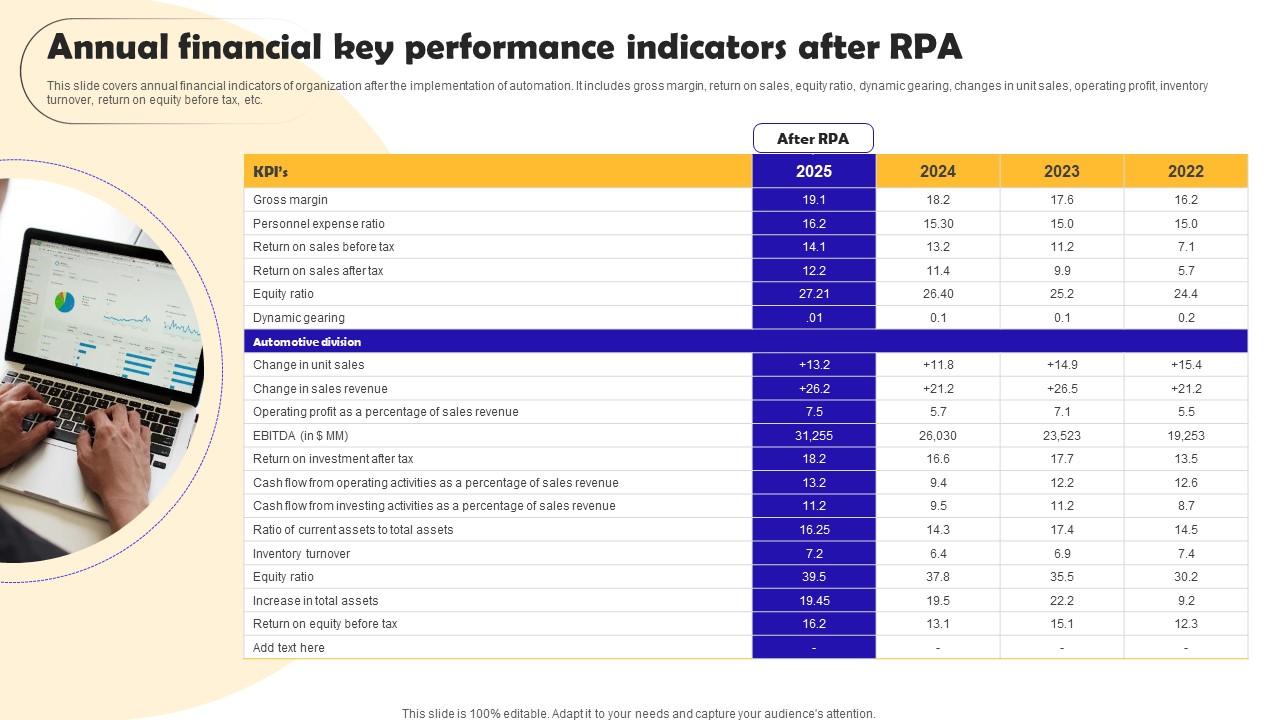
Annual Financial Key Performance Robotic Process Automation We can significantly improve operational efficiency, turnaround time, financial performance, and patient satisfaction. this synergy is the cornerstone of an effective pa process. Prior authorization automation presents a substantial opportunity for healthcare organizations to improve their financial performance. by harnessing the power of automation, providers can streamline the prior authorization process, reduce denials, and enhance the revenue cycle. Making prior authorization faster using automation can help a medical practice’s cash flow. with quicker approvals, practices can bill more accurately and get paid sooner. Automated prior authorization improves financial performance and staff efficiency. nearly all interviewed organizations have seen improved financial outcomes and or staff efficiency.
Prior Authorization Automation Services Streamline Authorizations Making prior authorization faster using automation can help a medical practice’s cash flow. with quicker approvals, practices can bill more accurately and get paid sooner. Automated prior authorization improves financial performance and staff efficiency. nearly all interviewed organizations have seen improved financial outcomes and or staff efficiency. Ai agents learn from the outcomes. they’re not just repeaters of static instructions. they adapt over time, improving accuracy and helping staff work more efficiently. just as importantly, they. Automating prior authorizations can help reduce denied claims, decrease errors and streamline the process. One healthcare process that could potentially be improved through the application of ai is prior authorization (pa). pa is a core administrative process in which payers require providers to obtain preapproval to administer a service or a medication as a condition of coverage. Ama news wire inside payers' latest plans to streamline prior authorization jul 14, 2025 with state and federal policymakers eyeing restrictions on health insurers’ use of the care delaying cost control process of prior authorization, the nation’s biggest carriers are pledging anew to make changes on a voluntary basis.

The Growing Burden Of Prior Auth Infographic Akasa Ai agents learn from the outcomes. they’re not just repeaters of static instructions. they adapt over time, improving accuracy and helping staff work more efficiently. just as importantly, they. Automating prior authorizations can help reduce denied claims, decrease errors and streamline the process. One healthcare process that could potentially be improved through the application of ai is prior authorization (pa). pa is a core administrative process in which payers require providers to obtain preapproval to administer a service or a medication as a condition of coverage. Ama news wire inside payers' latest plans to streamline prior authorization jul 14, 2025 with state and federal policymakers eyeing restrictions on health insurers’ use of the care delaying cost control process of prior authorization, the nation’s biggest carriers are pledging anew to make changes on a voluntary basis.
Comments are closed.