Automating The Prior Authorization Process

Automating Prior Authorization Akasa Our suite of solutions creates a comprehensive, end to end authorization platform that streamlines the critical functions of the authorization process and empowers providers and payers to manage prior authorizations more effectively. By understanding your current process, identifying key areas for automation, choosing the right ai solution (perhaps exploring the fully autonomous, fully agentic ai offered by magical), and following a step by step implementation and optimization approach, you can transform your prior authorization workflow from a frustrating burden into an.
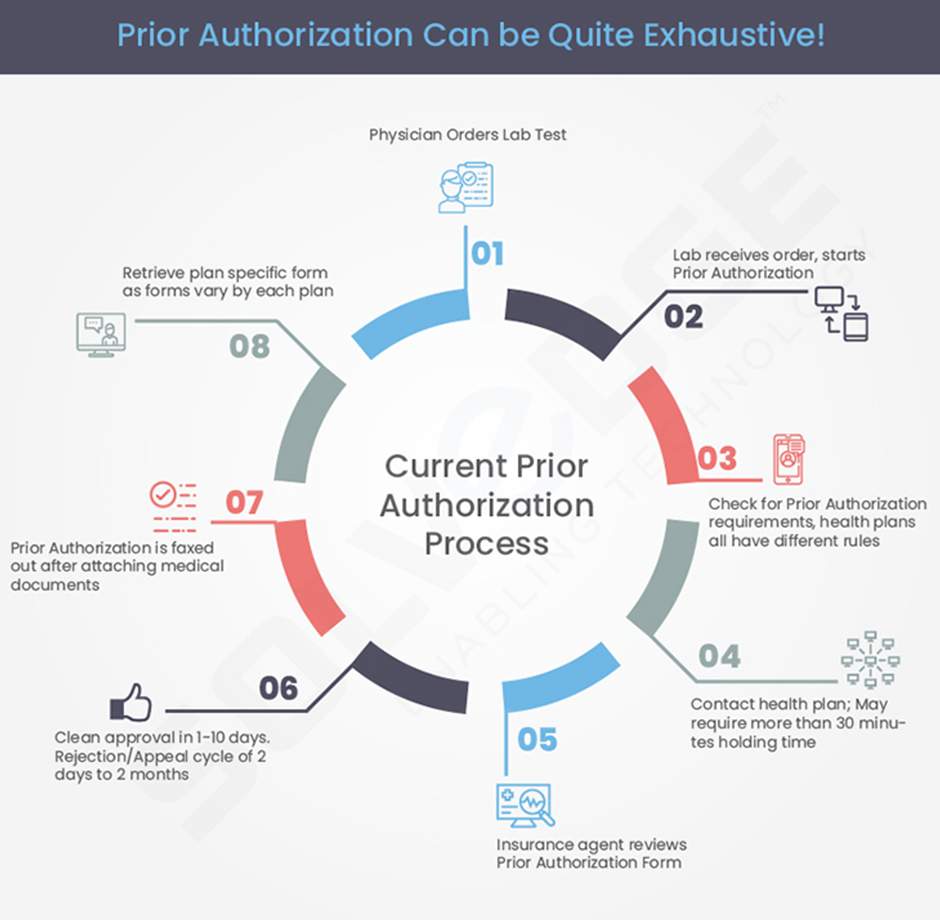
Cms S Rule On Automating Prior Authorization A Deep Dive As of interest in the automation of prior authorization context what considerations regarding potential benefits or challenges of au. Despite the many benefits of pa, the process itself is complex and can lead to additional administrative burden for providers and delayed access to care for patients. that’s why we have worked to simplify prior authorization through ongoing strategic technology investments and process improvements. One healthcare process that could potentially be improved through the application of ai is prior authorization (pa). pa is a core administrative process in which payers require providers to obtain preapproval to administer a service or a medication as a condition of coverage. Let’s dig deeper into the case for automating prior authorization, as well as details on how automation works for pas and how model providers are already streamlining prior authorization using automation.

Automating The Prior Authorization Process Enhances The Healthcare One healthcare process that could potentially be improved through the application of ai is prior authorization (pa). pa is a core administrative process in which payers require providers to obtain preapproval to administer a service or a medication as a condition of coverage. Let’s dig deeper into the case for automating prior authorization, as well as details on how automation works for pas and how model providers are already streamlining prior authorization using automation. Explore 5 leading ai tools easing prior authorization. discover how healthcare providers save time, cut costs, and improve patient care efficiency. In this article, we’ll break down the automation journey, tools involved, and key considerations for healthcare providers looking to streamline their pa workflows. traditionally, prior authorization involves:. Eighteen minutes are saved per prior authorization request, which for an average sized health plan unlocks tens of thousands of hours each month, that enables clinical care teams to shift from. Learn how automating prior authorizations reduces delays, cuts denials, and saves staff time, unlocking faster care and improved revenue capture for your organization.

Automating The Prior Authorization Process Enhances The Healthcare Explore 5 leading ai tools easing prior authorization. discover how healthcare providers save time, cut costs, and improve patient care efficiency. In this article, we’ll break down the automation journey, tools involved, and key considerations for healthcare providers looking to streamline their pa workflows. traditionally, prior authorization involves:. Eighteen minutes are saved per prior authorization request, which for an average sized health plan unlocks tens of thousands of hours each month, that enables clinical care teams to shift from. Learn how automating prior authorizations reduces delays, cuts denials, and saves staff time, unlocking faster care and improved revenue capture for your organization.

Automating The Prior Authorization Process Enhances The Healthcare Eighteen minutes are saved per prior authorization request, which for an average sized health plan unlocks tens of thousands of hours each month, that enables clinical care teams to shift from. Learn how automating prior authorizations reduces delays, cuts denials, and saves staff time, unlocking faster care and improved revenue capture for your organization.
Comments are closed.