5 Tips For Submitting Prior Authorization Requests

5 Tips For Submitting Prior Authorization Requests Recondo Technology, a revenue cycle management solutions company based in Denver, will host a complimentary webinar on how hospitals can automate prior authorization requests to payers The 2 Administrative Burden on Providers Healthcare providers, particularly those in smaller practices, face a significant administrative burden in managing prior authorization requests

5 Tips For Submitting Prior Authorization Requests Many prior authorization requests are processed in one to three business days, especially for standard medications with properly completed paperwork Some insurance companies may take up to five 5 takeaways from health insurers’ new pledge to improve prior authorization Mehmet Oz, current administrator of the Centers for Medicare & Medicaid Services, speaks at an election night rally in Delays in prior authorization can in turn delay treatment — and therefore relief — for suffering patients (While the majority of prior authorization requests are approved, the share of denials is The 5 Most Denied Prior Authorization Requests and How to Prevent These Denials Robert Neaderthal, MD, MBA Disclosures September 17, 2019 0

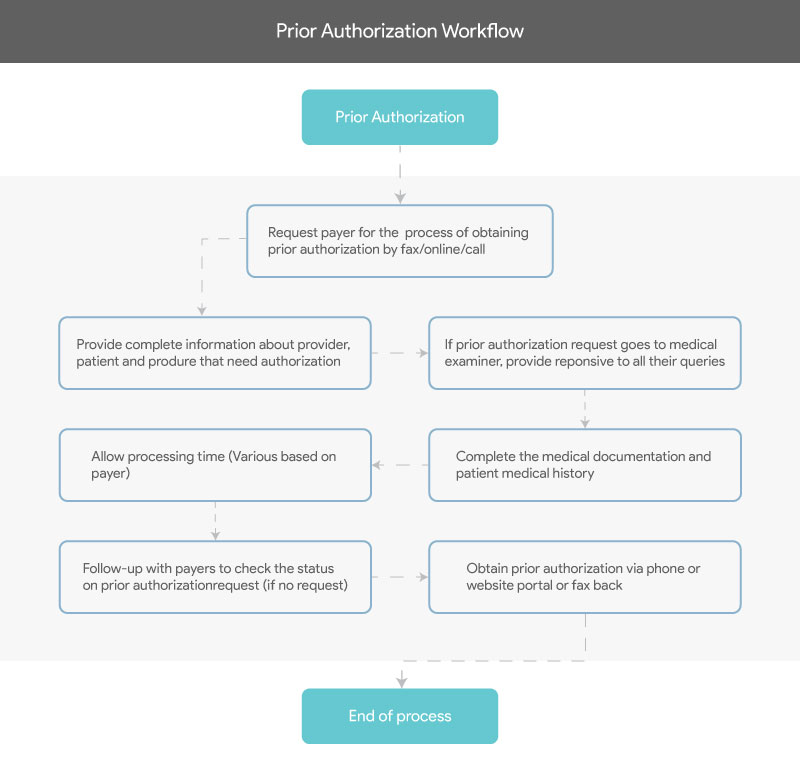
Submitting Requests For Prior Authorization Delays in prior authorization can in turn delay treatment — and therefore relief — for suffering patients (While the majority of prior authorization requests are approved, the share of denials is The 5 Most Denied Prior Authorization Requests and How to Prevent These Denials Robert Neaderthal, MD, MBA Disclosures September 17, 2019 0 Your insurer will then decide whether or not to cover your medicine Keep in mind: If you’re approved, a prior authorization only lasts for a set period of time A prior authorization can expire The use of AI in making prior authorization decisions isn't new — and it will probably continue to ramp up, with insurers pledging Monday to issue 80% of prior authorization decisions "in real Prior authorization isn’t going anywhere Health insurers will still be allowed to deny doctor-recommended care, which is arguably the biggest criticism that patients and providers level against Many prior authorization requests are processed in one to three business days, especially for standard medications with properly completed paperwork Some insurance companies may take up to five

Prior Authorization Refers To The Eligibility Verification Method That Your insurer will then decide whether or not to cover your medicine Keep in mind: If you’re approved, a prior authorization only lasts for a set period of time A prior authorization can expire The use of AI in making prior authorization decisions isn't new — and it will probably continue to ramp up, with insurers pledging Monday to issue 80% of prior authorization decisions "in real Prior authorization isn’t going anywhere Health insurers will still be allowed to deny doctor-recommended care, which is arguably the biggest criticism that patients and providers level against Many prior authorization requests are processed in one to three business days, especially for standard medications with properly completed paperwork Some insurance companies may take up to five Health insurers issue millions of denials every year, though most prior authorization requests are quickly, sometimes even instantly, approved The use of AI in making prior authorization decisions

Fillable Online Submitting Requests For Prior Authorization Fax Email Prior authorization isn’t going anywhere Health insurers will still be allowed to deny doctor-recommended care, which is arguably the biggest criticism that patients and providers level against Many prior authorization requests are processed in one to three business days, especially for standard medications with properly completed paperwork Some insurance companies may take up to five Health insurers issue millions of denials every year, though most prior authorization requests are quickly, sometimes even instantly, approved The use of AI in making prior authorization decisions
5 Key Strategies To Effectively Streamline And Overcome Prior Health insurers issue millions of denials every year, though most prior authorization requests are quickly, sometimes even instantly, approved The use of AI in making prior authorization decisions
Comments are closed.